
In the complex and changing landscape of modern healthcare, multidisciplinary team (MDT) meetings stand as a critical cornerstone in the pursuit of improved patient care and outcomes.
In this blog, we provide a comprehensive overview of MDT meetings so that anyone can understand how they work, why we need them, the challenges, and solutions of MDTs, etc.
Table of contents:
- Historical context of MDT meetings
- The value of MDT meetings
- The evolution of MDT meetings
- What does the digitally supported MDT Meeting process look like?
- The 4 challenges of non-digitally supported MDT meetings
- How can digital solutions improve the quality of MDT meetings?
- Example of a comprehensive digital solution: Vitaly MDT solution
- The success story of regional MDT meetings
- Final thoughts
Historical context of MDT meetings
To truly appreciate the role and significance of MDT meetings, it is essential to understand their historical context and evolution within healthcare.
The concept gained significant traction in the early 20th century, notably in the field of oncology, to deal with logistical, resource, and patient data-sharing challenges. MDTs became the gold standard of cancer care.

This collaboration brought together oncologists, surgeons, radiologists, pathologists, and other experts to collaboratively review cancer cases and devise treatment strategies.
The success of tumour boards in improving cancer patient outcomes paved the way for the broader adoption of MDT meetings across various medical specialities.
Now that we understand the background better, let’s explore why are MDT meetings so valuable and beneficial for healthcare organisations and patients.
The value of MDT meetings
MDTs present a clinical workflow for sharing and presenting relevant medical data aiming to unite care professionals from different disciplines and institutions to jointly decide upon the best possible treatment.
In this way decisions taken for the patients are based on all available information and scientific evidence where each member can provide their specific expertise.
Due to many proven benefits of such collaborative models, MDTs evolved into cross-organisational practice with the goal of providing more accurate treatment recommendations, multidisciplinary evaluation and adherence to clinical guidelines among all participating institutions.
Moreover, some of the most common benefits of MDTs are:
- Positively influencing clinical decision-making
- Inducing better team performance after case discussion
- Inducing more accurate diagnoses
- Increasing screening rates for clinical trials
- Reaching faster collaborative decisions, avoiding treatment delays
The evolution of MDT meetings
MDT meetings have undergone a remarkable transformation over the years, adapting to the dynamic field of healthcare.
This evolution has been shaped by technological advancements, the diversification of MDT specialities and a growing emphasis on patient-centred care.
Let’s explore some examples.
1. Technological Advancements:
Electronic Health Records (EHRs):
The adoption of EHRs has revolutionised the way patient data is accessed and shared during MDT meetings. Digital records allow for real-time updates and seamless communication among team members, ensuring all stakeholders can access the most current patient information.

Telemedicine and Video Conferencing:
The advent of telemedicine technologies has extended the reach of MDT meetings beyond geographical constraints. Virtual MDT meetings, facilitated by digital platforms, enable participation by experts from remote locations, enhancing collaboration and accessibility.
Decision Support Systems:
Advanced decision support tools have become integral to MDT meetings. These systems assist in data analysis, treatment planning and predicting outcomes, providing valuable insights to the MDT.
2. Diverse Specialties and Types of MDTs:
Expansion into Various Medical Specialties:
While MDT meetings initially gained prominence in oncology, their application has expanded into diverse medical specialities. Today, MDTs can be found in cardiology, neurology, paediatrics, orthopaedics, and more. Each brings its unique expertise to the collaborative decision-making process.
Specialised MDTs:
In addition to general MDTs, specialised teams have emerged to address specific healthcare challenges. Examples include paediatric MDTs for childhood cancer care, trauma MDTs for managing severe injuries and heart teams for complex cardiac cases.
3. Patient-Centred Care:
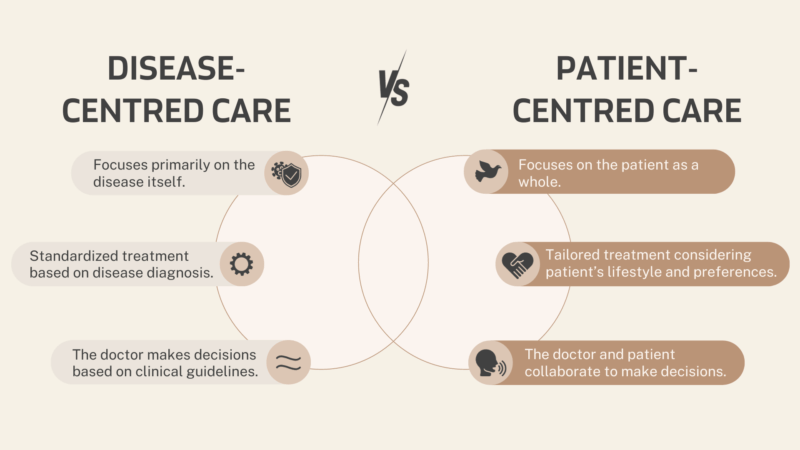 Visualised after the Health Standards Organisation blog.
Visualised after the Health Standards Organisation blog.
Incorporating Patient Preferences:
Modern MDT meetings increasingly emphasise patient-centred care. Patients are encouraged to actively participate in meetings, share their preferences, and engage in shared decision-making. Their input is considered vital in tailoring treatment plans.
Interdisciplinary Education:
There is a growing focus on training healthcare professionals to work effectively in MDT settings. Interdisciplinary education programs promote collaboration, communication skills, and the ability to navigate diverse perspectives, all essential for patient-centred care.
4. Quality Improvement and Outcomes Measurement:
Data-Driven Decision-Making:
MDT meetings have started to include analytics, with an emphasis on measuring outcomes and tracking the impact of decisions on patient care. Continuous quality improvement is a central theme, and teams can use data to refine their processes.
As healthcare continues to evolve, MDT meetings will remain at the forefront of interdisciplinary collaboration, ensuring that patients receive the best possible care from a team of experts working seamlessly together.
What does the digitally supported MDT Meeting process look like?
For MDT meetings to achieve their full potential, it is crucial to adhere to a structured and well-defined framework.
In this section, we will delve into the core elements of the MDT meeting process to get a better understanding of how they work. 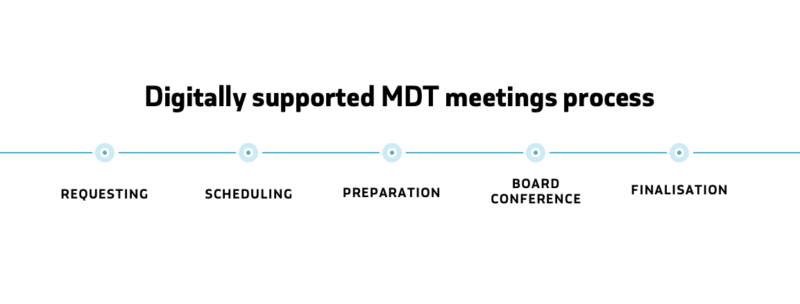
1. Requesting phase
The process begins when a healthcare professional identifies a complex medical case that could benefit from the collective expertise of an MDT.
The patient’s medical history, diagnostic reports, and relevant information are collected for presentation.
The MDT coordinator, often a nurse or administrative staff, collaborates with the referring healthcare professional to develop the meeting agenda. Cases are prioritised based on urgency and complexity.
Clear objectives for each case are established.
2. Scheduling Phase
The MDT coordinator schedules the meeting at a time and frequency appropriate for the speciality and the cases to be discussed.
The role of the scheduler serves as a gatekeeper to review all information provided by the requester. This helps to ensure the quality of data is relevant to the MDT discussion.
Invitations are sent to MDT members, ensuring attendance and representation from various specialities.
3. Preparation phase
After the case is scheduled for the board, all MDT participants receive a notification about a new patient in review.
They can all access the information along with consultation material provided by the requester, which helps them to efficiently prepare and share their recommendations before the meeting.
4. Board conference phase
During the meeting, the referring healthcare professional presents the case, providing essential information, including the patient’s medical history, test results, and current treatment.
Radiological images, pathology reports, and other relevant data are shared for discussion.
MDT members engage in collaborative discussions, sharing their perspectives and expertise. The goal is to arrive at a consensus on the diagnosis, treatment plan, and overall management of the case.
A shared decision-making process takes place, emphasising the integration of various specialist opinions. Treatment options are considered, and the pros and cons of each approach are weighed.
Based on the discussion and consensus, a comprehensive treatment plan is developed, tailored to the patient’s unique needs. The plan may include surgery, medication, therapy, or a combination of interventions.
At the time of the meeting, the Scribe writes a preliminary report for each case separately, which is then shared with the chair for finalisation.
5. Finalisation phase
In the finalisation phase, the chair can make revisions and finalise the report. Within the last step all board members get notified that the final report is ready and accessible.
The report can be published to the patient’s electronic record and made accessible to other healthcare professionals.
The referring healthcare professional implements the agreed-upon treatment plan. The patient’s progress is closely monitored, and follow-up MDT meetings may be scheduled to review outcomes and adjust the treatment plan as necessary.
But it’s safe to say the process doesn’t always go so smoothly. Let’s explore why.
The 4 challenges of non-digitally supported MDT meetings

Just like any significant healthcare initiative, MDT meetings have their own set of challenges. Let’s address some of these challenges and explore how integrating digital solutions can be the bridge to overcoming them, ultimately leading to improved patient care and outcomes.
Challenge 1: Administrative burden
One of the significant hurdles in MDT meetings is the excessive administrative work. These meetings often entail extensive paperwork, agenda management, and data organisation, which can consume considerable time for healthcare professionals. This administrative burden diverts their attention away from patient care.
Challenge 2: Unequal quality of care
A prevalent logistical and local challenge in MDT meetings lies in the unequal distribution of quality care. Geographic disparities restrict access to the best specialists for many individuals, creating a barrier to receiving optimal healthcare.
This issue highlights the need for solutions that bridge geographical gaps and ensure equitable access to expertise, regardless of one’s location.
Challenge 3: Inefficient data exchange
Another significant hurdle faced by MDT meetings is the inefficiency in data exchange. Traditional methods often involve cumbersome processes, leading to delays, errors, and potential oversights in patient information.
Streamlining data exchange is crucial for MDTs to operate seamlessly, enabling quick access to comprehensive patient data and facilitating informed decision-making.
Challenge 4: Ensuring attendance and engagement
Ensuring that all MDT members attend and actively engage in meetings can be challenging. This challenge arises from varying work schedules, the demands of other patient care responsibilities, and differing levels of engagement and interest among team members.
It’s crucial that all relevant specialists actively participate and contribute to the decision-making process to ensure a comprehensive evaluation of complex cases.
Addressing these challenges requires a combination of digital technology adoption, clear communication protocols, and effective leadership.
Digital technology has the potential to address most of the faced challenges. Let’s see why.
How can digital solutions improve the quality of MDT meetings?

MDT meetings offer a comprehensive range of benefits in healthcare, but without the proper support from digital technologies, the potential and benefits are severely limited.
The healthcare sector has always been cautious in adopting digital technology due to the sensitivity and complexity of the field. However, there is no longer a question of whether the healthcare sector should embrace digital transformation.
Here are some advantages of digitally supported multidisciplinary team meetings, aligning the healthcare sector with the demands of the digital age.
1. Improved Workflow and Capacity:
Digital support enhances the efficiency of MDT meetings, allowing healthcare professionals to review cases, make decisions, and implement treatment plans more rapidly. One of the main goals is to relieve clinicians as much as possible, making their work easier.
This increased workflow efficiency translates into the ability to treat more patients, ultimately reducing waiting times and expanding the healthcare system’s capacity to address a broader patient population.
2. Reduced Administrative Burdens:
Digital platforms made for MDT meetings streamline administrative tasks, allowing clinicians to focus on patient care rather than paperwork. Automating routine tasks, such as data entry and record-keeping, helps minimise the burden.
3. Cost Savings:
By reducing the need for physical meetings and travel and allocating resources more efficiently by optimising meeting schedules, ensuring appropriate team member attendance, and reducing the time spent on administrative tasks, healthcare organisations can use their resources more effectively.
4. Patient Engagement and Empowerment:
Digital platforms offer opportunities for patient engagement and empowerment within MDT meetings.
Patients can have direct access to their health records and treatment plans, fostering a sense of ownership and involvement in their care.
This participatory approach often leads to more satisfied and informed patients, improving health outcomes.
5. Collection and analysis of data:
Digitally supported MDT meetings facilitate the collection and analysis of data related to patient outcomes and the decision-making process.
This data-driven approach empowers healthcare institutions to implement continuous quality improvement initiatives, refining processes and enhancing the quality of care over time.
Example of a comprehensive digital solution: Vitaly MDT solution
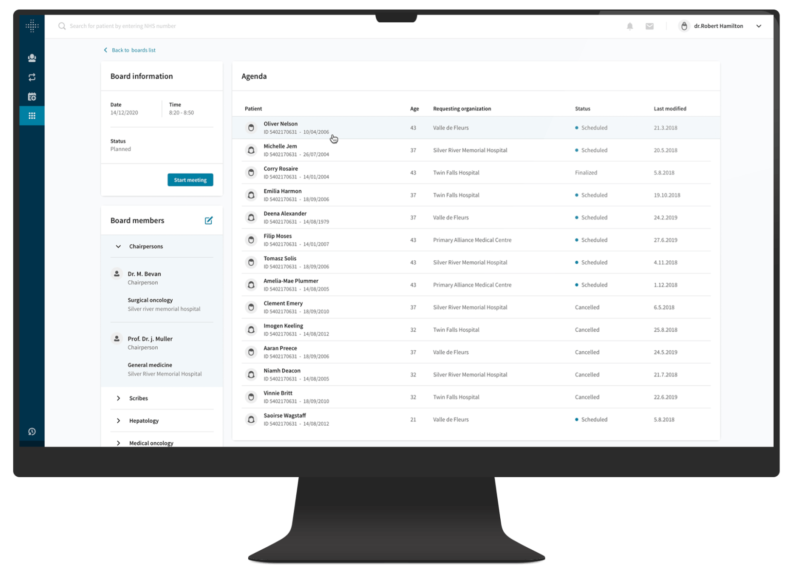
It goes without saying that a comprehensive digital solution is the next step for most healthcare organisations to adjust to our society’s rising demands. But what does such a solution look like, and what should it offer?
With Vitaly, integrated care systems and providers can support collaborative decisions through MDT meetings, engage patients waiting for treatment, and then take individuals through the outpatient, treatment, and post-treatment journey from a single platform.
There are a variety of capabilities to help achieve digital transformation successfully. Let’s take a look at some of them.
Streamlined protocol-driven workflows
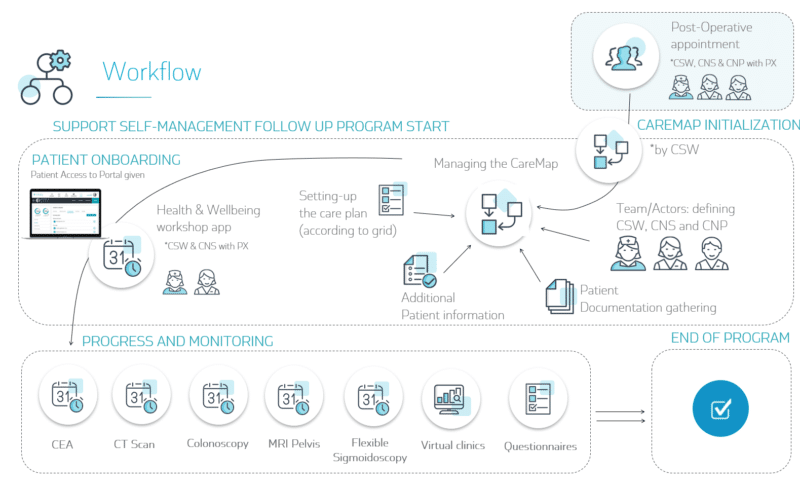
Vitaly MDT solution incorporates protocol-driven workflows that seamlessly integrate with existing MDT processes.
These workflows are adaptable to any range of therapeutic areas, including cancer care, mental health, chronic diseases, and pediatric care.
Such streamlining ensures that MDT meetings are conducted efficiently while adhering to established protocols.
Customised dynamic forms
Within the solution, a dynamic form creator is available for customisation to meet diverse requirements.
These customised forms are seamlessly integrated into a patient’s electronic health record, guaranteeing structured and comprehensive documentation of decisions and recommendations.
Patient data
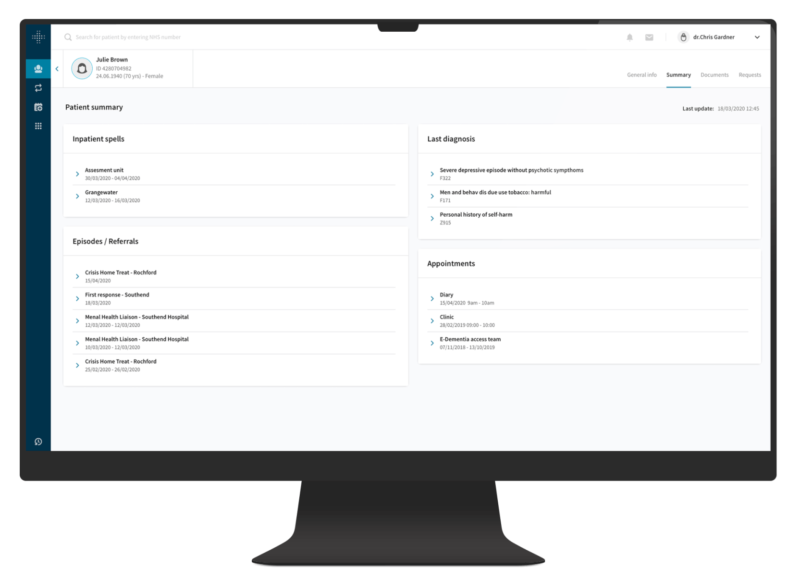
Our MDT solution is capable of aggregating relevant patient data from various health information sources.
Data is vital for prompt reviews, establishing a thorough medical background, and evaluating potential treatment options. A comprehensive patient overview improves the quality of discussions during MDT meetings.
Video session hosting and facilitation

Vitaly solution provides functionalities for planning, scheduling, hosting, and facilitating video sessions.
This streamlines the progression of patients’ requests, from submission to scheduling, and supports remote participation, ensuring that all essential participants can actively engage in the review process.
Error minimisation and preparation
Vitaly solution oversees the preparation of complex cases before MDT meetings, assisting the team in aligning and preparing for decision-making.
This proactive approach minimises errors and ensures that discussions are focused and productive.
Interoperability and standards
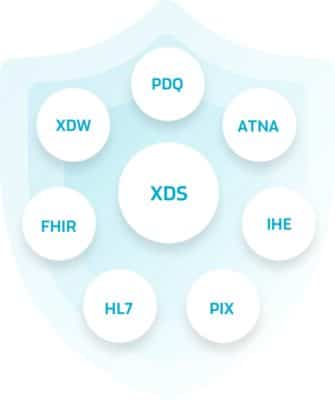
Vitaly solution facilitates seamless data sharing and communication between various healthcare systems by leveraging the adoption of interoperability profiles and standards, such as :
- IHE XTB-WD,
- IHE XBeR-WD,
- FHIR,
- openEHR
- etc.
Interoperability ensures seamless data sharing, reduces data silos, enhances communication, ensures compliance and security, and future-proofs the solution.
Specialisation for various MDT specialties
The solution is adaptable to meet the unique needs of MDTs across various specialities, ranging from oncology and cardiology to child and adolescent care, mental health, obstetrics, and more.
Its flexibility and versatility should allow for any future scalings and ensure that it can cater to the specific requirements of each clinical MDT group.
Built-in analytics and reporting

Vitaly solution includes built-in analytical features that provide real-time performance insights and participation data.
This further aids healthcare organisations to see clearly if their service is operating efficiently and extract the relevant indicators for continuous improvement of processes and quality of care.
It’s easier than ever to track key metrics that help promptly identify trends and pitfalls on what works and where they can still improve the quality of patient care, the productivity of staff, and create an overall positive experience through transparent data-sharing.
The success story of regional MDT meetings
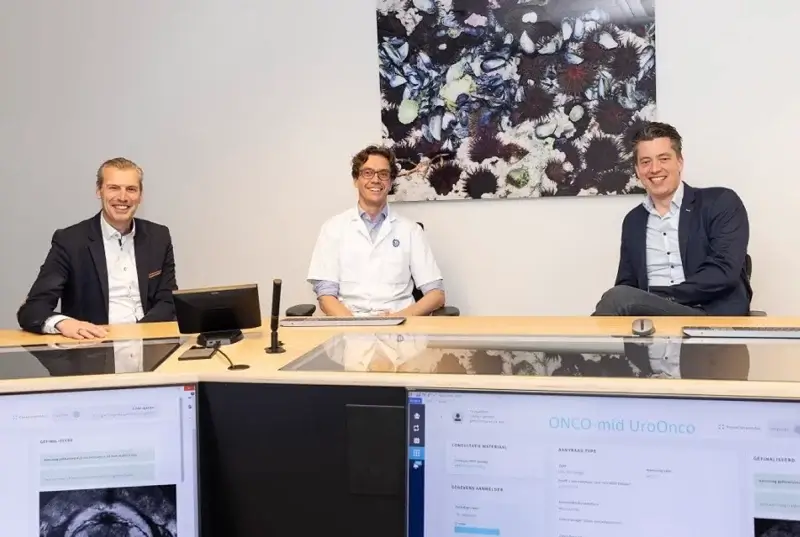
The DDMN, often referred to as “Data Dellen Midden Nederlands,” is one of the most successful stories when it comes to integrating a comprehensive digital MDT solution to enhance their regional MDT meetings.
It is a pioneering healthcare collaboration between 6 Oncomid hospitals based in the central Netherlands, which is an initiative that is a part of the Dutch national program, “The Right Care in the Right Place”.
This regional initiative aimed to improve the quality of care for cancer patients in the region by increasing clinical efficiency, improving user satisfaction and enhancing the automated data exchange for patients referred to regional MDT meetings.
It includes a complete ecosystem of IT partners who support real-time data exchange, security, and integration based on open standards.
From Paper-Based to Digital Excellence
In the not-so-distant past, MDT meetings at DDMN were conducted using traditional paper-based systems. These meetings often involved extensive paperwork, the use of old CD-ROMs, manual documentation, and the exchange of physical files.
The turning point for DDMN came with the integration of Vitaly MDT solution. Listen to the story of dr Koos van der Hoeven, Oncomid’s chairman, where he talks about what happened after transitioning to digitally supported MDT meetings.
Arjo Boendermaker, Project Lead at DDMN, further explains and shares his insights on how they saved valuable time for each registered patient.
By embracing digital technology, DDMN witnessed a transformation in its MDT meetings. The transition to fully integrated digital MDT meetings led them to improved patient care, enhanced communication and collaboration among healthcare professionals, efficient resource allocation, and reduced administrative burdens.
Their journey from traditional to digital MDT meetings exemplifies the profound impact that technology can have on healthcare, ultimately leading to better patient outcomes and a more promising future for the entire healthcare system.
You can learn more about DDMN’s integration journey by clicking here.
Final thoughts
Our journey through the world of MDT meetings and their evolving role in healthcare is nothing short of remarkable.
These meetings, once confined to specific medical disciplines, have grown to become powerful instruments of interdisciplinary collaboration, with technology as a driving force.
But this is not the end of the story. The narrative continues, with healthcare professionals and organisations shaping a future towards improved patient care, seamless collaboration, and heightened efficiency.
This is our mission, to help our health care systems deal with the ever-rising demands. Our Vitaly platform is built for connection and collaboration at all levels and can deliver truly transformative outcomes.
Let’s all work together to build a world where everyone receives the quality care they deserve!